[ad_1]
What your doctor is reading on Medscape.com:
APRIL 28, 2020 — Calendar year 2020 will be remembered for the COVID-19 pandemic, handwashing, and social distancing. As I write this, clinical trials are underway to test both therapeutics and vaccine candidates against SARS-CoV-2. One area that has been understudied but requires a fresh look is the use of extracorporeal therapy such as plasmapheresis.
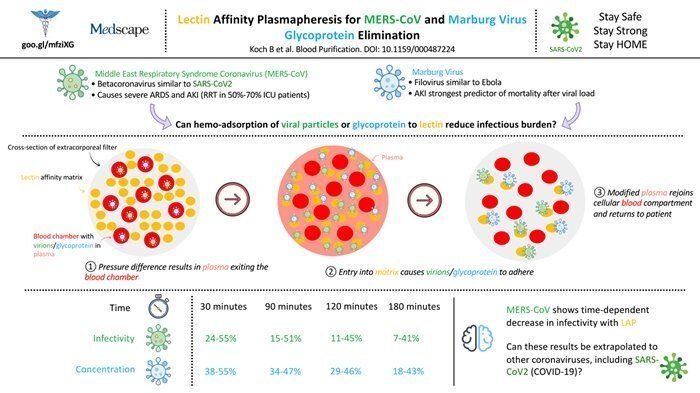
Plasmapheresis uses modified dialysis filters to bind key components of viral replication or the virus itself, with the goal of returning uninfected plasma to the patient. This strategy has been studied in the Ebola and Middle East respiratory syndrome (MERS) epidemics. Nearly all of those studies were small and required tremendous resources (eg, filter, dialysis pumps and electricity, anticoagulation).
One such in vitro study tested whether a lectin-embedded filter could reduce infectivity of MERS-CoV. Previous in vitro studies have shown that lectin can bind to various surface glycoproteins of MERS-CoV.
As outlined in the infographic above, blood infected with MERS-CoV was perfused through the filter and passed through a lectin affinity matrix, where the virions are bound to the lectin, resulting in virus-free plasma. A small number of timed experiments show that infectivity of MERS-CoV decreases the longer the blood is perfused through the lectin affinity matrix. In just 30 minutes, infectivity drops nearly 50%; and after 3 hours of treatment, infectivity can be as low as 7%.
Admittedly, studies involving extracorporeal therapies are very small, but they offer another therapeutic option to treat viral epidemics. Deploying plasmapheresis will be difficult due to the amount and intensity of ancillary resources needed, but for a select group of critically ill patients this therapy may be more effective than a pharmacologic agent. The lectin affinity matrix has been studied only in MERS-CoV, but given the limited options for COVID-19, I’m not the only one suggesting that we consider extracorporeal therapies for critically ill SARS-CoV-2 patients.
With the focus on ventilator protocols and drug candidates, it’s important to increase awareness of this potential therapeutic option. And as with all potential treatments for COVID-19, we should test them in well-conducted research trials.
To find out what nephrologists are saying about extracorporeal therapies in COVID-19, visit #NephTwitter Archives.
Tejas Desai is a practicing nephrologist in Charlotte, North Carolina. His academic interests include the use of social media for physician, student, and patient education. He is the founder of NOD Analytics, a free social media analytics group that serves the medical education community. He has two wonderful children and enjoys spending time with them and his wife.