[ad_1]
What your doctor is reading on Medscape.com:
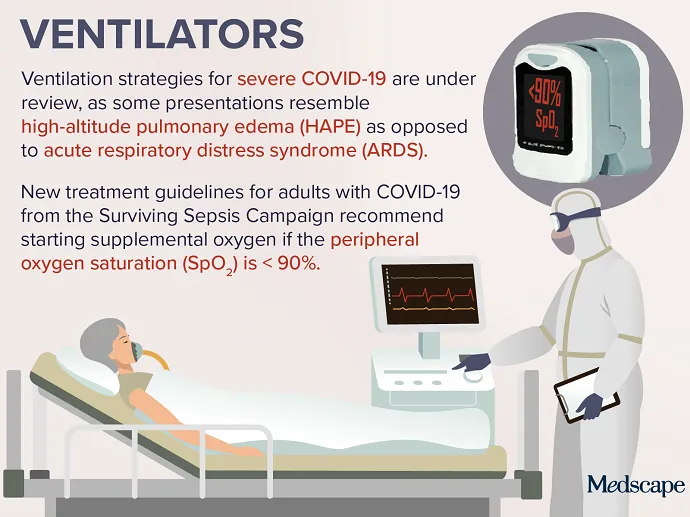
APRIL 16, 2020 — Controversy has emerged regarding the treatment of certain patients with severe COVID-19. Concerns about proper protocols and the rationing of care resulted in ventilators becoming the top trending clinical topic this week. Some physicians caring for patients with COVID-19 pneumonia are questioning whether standard respiratory therapy protocols for acute respiratory distress syndrome (ARDS) are the best approach, given that the disease may more closely resemble high-altitude pulmonary edema (HAPE) in some patients.
In a letter to the editor published in the American Journal of Respiratory and Critical Care Medicine on March 30, Luciano Gattinoni, MD, of the Medical University of Göttingen in Germany, and his colleagues suggest that protocol-driven ventilator use in COVID-19 pneumonia could be more harmful than helpful. Gattinoni and coworkers recommend that physicians should use the lowest possible positive end-expiratory pressure (PEEP) and gentle ventilation instead of high PEEP to “buy time with minimum additional damage.”
Cameron Kyle-Sidell, MD, a critical care physician in New York City, agreed with Gattinoni in an interview on the subject. He described seeing two different phenotypes in patients with COVID-19 pneumonia: one in which the lungs display high compliance and low elastance and another in which the lungs have low compliance and high elastance. Both Kyle-Sidell and Gattinoni are in support of changes to guidelines for the management of critically ill adults with COVID-19, which are scheduled to be published in Intensive Care Medicine. Those guidelines are from the Surviving Sepsis Campaign, a joint collaboration of the Society of Critical Care Medicine and the European Society of Intensive Care Medicine.
In addition to concerns about appropriate ventilation strategies, worries have arisen over the rationing of ventilators. Reports emerged that various US states were planning to ration use of ventilators and other crucial COVID-19 treatments on the basis of patient characteristics, including age, overall health, and disabilities. The director of Health and Human Services’ Office for Civil Rights issued a bulletin stating that patients with disabilities “should not be denied medical care on the basis of stereotypes, assessments of quality of life, or judgements about a person’s relative ‘worth’ based on the presence or absence of disabilities.”
Continued
As countries around the world face potential shortages of ventilators and other lifesaving treatments for patients with severe COVID-19, ethicists are weighing in on the issue. Arthur L. Caplan, PhD, reviewed around 70 policies from different hospital systems and highlighted key aspects. In addition to reiterating that no “categories of people” should be ruled out of receiving certain care, Caplan identified key factors in the quest to “save the most lives.” This included age, whether the individual is a healthcare worker, and significant underlying illness. He also suggested that “we may have situations where we have to take someone off who has been on for 8 or 9 days of ventilator support and isn’t responding, and we have someone who comes in who is young and otherwise healthy and looks like they would do better.”
A focus on ventilator use is likely to persist as COVID-19 cases continue to mount. Further refinement of protocols and guidance on rationing is eagerly anticipated.